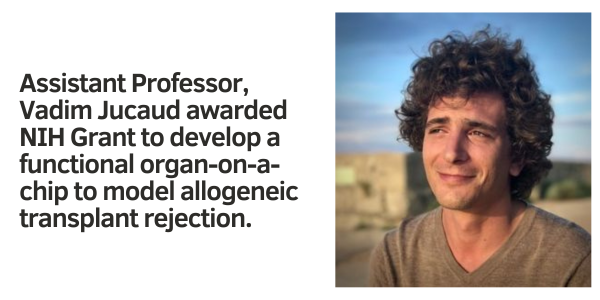
(LOS ANGELES) – Vadim Jucaud, Ph.D., Assistant Professor at the Terasaki Institute for Biomedical Innovation, has been awarded a grant from the National Institutes of Health to develop a functional organ-on-a-chip to model allogeneic transplant rejection. Such a model would allow the study of allograft tolerance and may ultimately lead to reducing organ transplant rejections without needing immunosuppressive drugs.
Organ transplantation is a lifesaving procedure for patients with end-stage organ disease. Over 145,000 organs per year are transplanted worldwide from organ donors to recipients. For these so-called allografts, recipients in need of an organ far outnumber organ donors; because of this, donated organs are precious, and every effort is made to minimize the risk of organ rejection by the recipient.
In addition to careful tissue matching and pre-transplant crossmatch testing, organ transplant recipients need to take immunosuppressive drugs for the remainder of their lives post-transplant. This presents a major challenge, as these drugs have the potential for serious side effects, which can lead to cancer, heart disease, kidney damage, and infections. Care must be given when treating such patients for comorbidities, and treatment for these additional diseases must be safely coordinated with their immunosuppressive regimens. Prohibitive costs and complicated medication regimens can also negatively affect patient compliance and post-transplant success.
Although it is thought that accurate tissue matching can help avoid allograft rejection, it is also hypothesized that certain tissue mismatches are less risky than others and that induction of immune tolerance and even spontaneous tolerance can be achieved.
The organ-on-a-chip model that Dr. Jucaud proposes may help to elucidate these events and how they can be maximized to benefit organ transplant patients. It can more accurately recapitulate allograft rejection than traditional models, allowing more rigorously controlled culture conditions and representation of a donor organ’s dynamics and functionality.
“We hope that our proposed model can help to improve immune tolerance and reduce the need for immunosuppressive drugs,” said Dr. Jucaud. “Simplifying these drug treatment regimens would greatly enhance the quality of life for solid organ transplant patients.”
The project funded by this grant would further the legacy of Dr. Paul I. Terasaki, Ph.D., a pioneer in the field of organ transplantation, who founded the original Terasaki Institute. Throughout his career, Dr. Terasaki devoted himself to research which would improve transplant outcomes and achieve the goal of each patient receiving “One Transplant for Life.”