(LOS ANGELES) – A collaborative team from the Terasaki Institute for Biomedical Innovation (TIBI) has developed a contact lens prototype that is specifically designed to prevent contact lens-induced dry eye (CLIDE). The lens alleviates this condition by facilitating tear flow in response to normal eye blinking. This approach can relieve the discomfort, visual impairment, and risk of inflammation experienced by millions of contact lens users suffering from CLIDE.
Of the 140 million contact wearers worldwide, 30%-50% suffer from CLIDE. The problem arises from the insufficient flow of tears from the contact lens's outer surface to the surface behind the lens. This leads to excessive tear evaporation and all the problems associated with CLIDE.
Current treatments for this condition include rewetting drops, gels, or lubricants, more frequent lens replacement, or changes in the lens material. There are also eyelid treatments, such as eyelid massage and warm compresses. In more severe cases, physical stimulation of the tear glands may be utilized, as well as the use of punctum plugs, devices inserted into tear ducts to block drainage. Efficacy varies among these treatments, however, as well as potentially harmful accumulations of drugs in the body and the non-user-friendly methods that contribute to patient noncompliance.
There have also been previous attempts to use contact lenses in treating dry eye syndrome, such as graphene-coated lenses designed to minimize moisture loss and self-moisturizing lenses stimulated with metallic electrodes. But these methods are costly and impractical and may compromise patient safety and comfort.
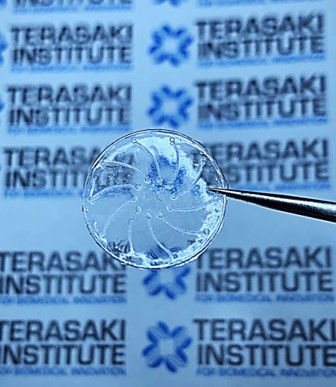
The TIBI team’s approach uses a contact lens design that incorporates microchannels to facilitate tear flow movement and flow so that dry eye can be avoided. This flow can be achieved by pressure applied by normal eye blinking so that no external devices are needed.
In fabricating their contact lens prototype, the team utilized a time-saving method – their lens mold was made from a silicone polymer mixture; this allowed for easy removal of the lens cast on it by gently bending the mold. Previous methods necessitated a twelve-hour soak in hot water to remove the lens. The approach resulted in high-quality, smooth microchannels, as well as lenses that could be thirty times thinner than previous lenses. A custom device was used to fabricate reservoirs at the ends of each microchannel for the inflow and outflow of liquids.
Innovative techniques were also utilized when encapsulating the microchannels in a sandwich-like assembly under a capping lens layer. Initially, the preparation of the two lens surfaces for stronger bonding dehydrated the lenses, causing them to curl. This problem was solved by affixing the two lenses to holders using water-soluble glue. This served not only to enable a more uniform bonding of the lenses but protected them from damage as well.
After rigorously testing their encapsulated microchannel lenses for stability and leakage, the lenses were subjected to a series of experiments using a device that the team designed to simulate a blinking eyelid. This device was integrated with the lens prototype to create artificial eyelid pressure on the lens to stimulate tear flow.
After various experiments, a configuration that proved effective was microchannels with square cross-sections arrayed in a novel circular pattern on the lens surface; this was compatible with the function and curvature of the lens and allowed for optimum liquid flow.
The team demonstrated a proof-of-concept validation of their lens’ ability to guide tear flow originating from the lens surface to the underside of the lens to combat dry eye syndrome. The team quantified these flows and established that the flows were driven by low-pressure levels like those from normal eye blinking. Further tests could be devised to test these lenses on animal models and in patients.
“The inventive methods that our team has employed bring a potential solution for millions of people,” said Ali Khademhosseini, TIBI’s Director and CEO. “It is the hope that we may extend our efforts to bring this solution to fruition.”
Authors are: Yangzhi Zhu, Elham Davoodi, Rohollah Nasiri, Shiming Zhang, Sourav Saha, Matthew Linn, Lu Jiang, Zhuohong Wu, Reihaneh Haghniaz, Jinjoo Kim, Marvin Mecwan, Heemin Kang, HanJun Kim, Vadim Jucaud, Mohsen Akbari, Anna Herland, Mehmet R. Dokmeci, Ehsan Toyserkani, Ali Khademhosseini.
This work was supported by Cooper Vision, Inc.
PRESS CONTACT
Stewart Han, This email address is being protected from spambots. You need JavaScript enabled to view it., +1 818-836-4393
Terasaki Institute for Biomedical Innovation
DOI: https://doi.org/10.1002/smll.202207017